Egg freezing is hardly new.
Egg freezing is a well-established medical procedure with decades of science and technology behind it. In fact, in the past five years alone, over 250 studies of oocyte cryopreservation (the technical term for egg freezing) have been published in medical journals.
Over thirty years of advancement
The first human birth from a frozen oocyte (egg) was reported in 1986. As a comparison, that same year, doctors inserted the first heart stent ever used on a human; today, over 1.8 million stents are placed every year. It was only one year prior, in 1985, that the automated external defibrillator (AED) was put into production—these life-saving devices are now ubiquitous on ambulances, in hospitals, and in schools. Suffice it to say that, in the world of medical development, 34 years means the difference between brand-new technology and everyday interventions.
Vitrification changed the game
Like all medical technology, egg freezing techniques have advanced significantly over the past three decades. The most noteworthy improvement was the development of vitrification, a flash-freezing method that lowers the chance that damaging ice crystals will form inside a frozen egg. Vitrification was first used on mouse embryos in 1985, but was later reintroduced for unfertilized human eggs in the mid-2000s. When using the old method of cryopreservation—known as slow freezing—only about 60% of eggs survived being frozen and then thawed. Vitrification changed the game, increasing egg survival rates to 90% or more.
From experimental to encouraging
Whenever a new medical procedure is introduced, it’s considered “experimental” until there’s a very strong base of evidence to support its regular use. Egg freezing was considered experimental until 2012, when the overwhelming evidence that the technology was both safe and effective—including the promising results of vitrification—convinced the industry’s leading organization, the American Society for Reproductive Medicine (ASRM), to change its classification. This change made egg freezing more widely available to more women.
ASRM issued an updated committee opinion on egg freezing in 2018 that reflected the vast body of research performed and evidence collected over the previous six years. This statement supported a change in terminology from “elective” or “social” egg freezing to “planned egg freezing,” representing the view that egg freezing is a proactive and preventative approach to fertility decline. It also acknowledged that egg freezing promotes social justice and gender equality by “reducing the obstacles women currently face because their reproductive window is smaller than men’s.”
The research is clear: egg freezing works.
One of the greatest misconceptions about egg freezing is that there’s not enough evidence to demonstrate that it works—or that success rates are disappointingly low. Neither could be further from the truth.
Freezing eggs preserves their health and their chance of success
Even before thousands of women began freezing their eggs for their own use, cryopreservation was common during egg donation, the process of using eggs from a healthy, fertile (often younger) woman to create an embryo(s) for use by another woman or couple. So, egg donation results can tell us a lot about how well frozen eggs fare when used for in vitro fertilization.
A randomized controlled clinical trial of over 600 egg donation recipients published in 2010 did just that: it compared pregnancy rates from “fresh” (AKA, never frozen) eggs used in IVF to pregnancy rates from vitrified and thawed eggs. This study found that freezing eggs didn’t reduce their quality or ability to create a healthy embryo. This means that freezing eggs at age 30 and using them 10 years later, for example, will give you the same chance of pregnancy at age 40 as if you’d done IVF at age 30—increasing your chance of success by over 200%.
2–12% success rates?
Many media outlets misleadingly state that egg freezing success rates are “2–12%,” reflecting a lack of understanding of how egg freezing really works. In fact, that statistic refers to the estimated live birth rate, per egg, for eggs frozen using old slow freezing technology. (With today’s vitrification technology, live birth rates are closer to 4–14% per egg according to ASRM.)
Let’s make one thing clear—no one freezes just one egg! Your chances of success will depend on two things: your age at the time of freezing, and how many eggs you freeze.
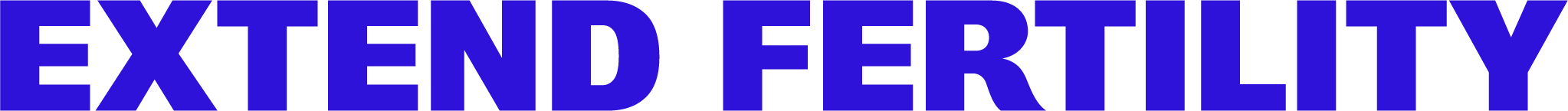
Chances of pregnancy can be over 70% for women who freeze before 35
Because egg health is age-dependent, success rates are higher for women who freeze at younger ages. In a report published in 2017, egg freezing researchers examined the results of 520 actual IVF cycles and the outcomes of genetic testing on over 14,000 embryos. They applied this data to create a model that uses the two most important factors in egg freezing success—age at the time of freezing, and how many eggs were frozen—to predict individual chances of egg freezing success.
According to this scientific model, women who freeze 10 eggs under age 35 have a 70% chance of having at least one baby using those eggs later on. If they freeze 20 eggs instead, that chance increases to 90%. Our own research of 1,100 egg freezing cycles revealed that women under 35 freeze, on average, 17 eggs in one cycle. So, for those who freeze young enough, success with frozen eggs is highly likely.
Like anything in life, there are no guarantees—but the science supporting egg freezing success is sound and strong. Egg freezing is an evidence-based treatment and a smart, proactive way to preserve fertility for the future.
Egg freezing is conclusively safe.
While there is some risk inherent in any medical procedure, egg freezing uses the same tried-and-true medications and procedures utilized for in vitro fertilization for decades, which have bountiful research supporting efficacy and safety for both the women who undergo the procedure and the offspring who result from it.
Fertility medications don’t increase risk of cancer
A comprehensive review of over 50 different studies looking at the connection between fertility medications and cancer concluded that fertility treatments “do not increase the risks of invasive ovarian cancer, malignant melanoma or cancers of the endometrium, cervix, breast, thyroid or colon.” One especially well-structured study tracked nearly 20,000 women who had taken fertility medications, monitoring their health over a period of 21 years, and found that breast cancer risk was no different than that of the general population.
Freezing eggs doesn’t appear to affect the health of future babies created from those eggs
A study of over 900 babies born from frozen eggs determined that there’s no increased risk of birth defects when compared to the general population. Additionally, long-term offspring health has been shown to be unaffected by the use of assisted reproductive technology; at least eight studies have examined the postnatal development of children born from IVF and found no significant differences from naturally conceived children.
The chance of serious side effects is extremely low
Less than 1% of women taking fertility medications develop severe ovarian hyperstimulation syndrome (OHSS), a condition in which the ovaries respond too strongly to the medications. OHSS can be almost entirely prevented with careful monitoring and state-of-the-art medication protocols.
The chance of complications during the egg retrieval is even lower. This quick outpatient procedure is minimally invasive, with the chance of infection around .5% and the chance of anesthesia complications hovering around 1 in 300,000 patients (that’s less than your chance of being in a plane crash, for comparison).
Fertility decline with age is scientific consensus.
One of the most pervasive myths about egg freezing is that it’s not necessary because fertility doesn’t really decline that much with age. This is unfortunately reinforced by stories of celebrities having babies at age 45 and beyond—with little discussion of the medical technology (and expense!) it took to get there.
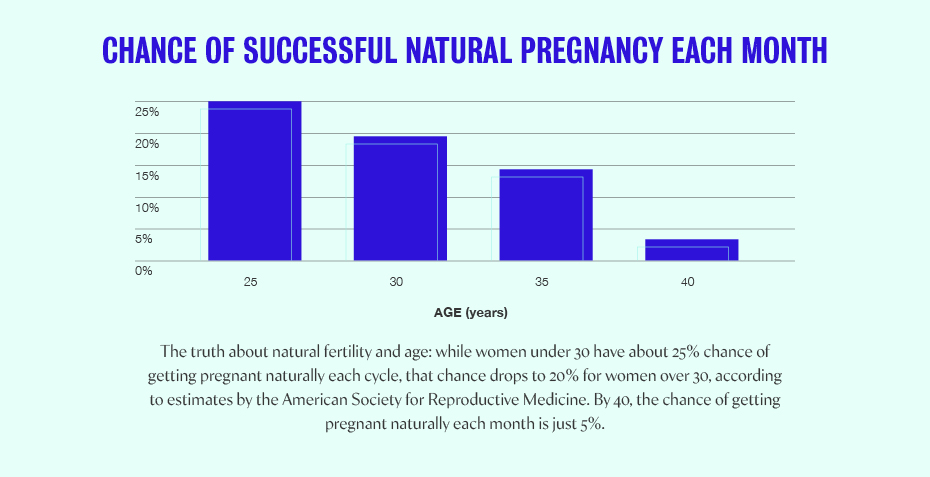
The truth is that your chance of natural pregnancy at age 40 is a quarter of what it is at age 30, and even powerful infertility treatments like IVF can’t entirely compensate for this decline. As you age, the number of eggs in your ovaries decreases and your percentage of unhealthy eggs increases—that’s why we see steadily increasing rates of infertility with age. There’s an entire body of thorough evidence demonstrating that age is, by far, the largest factor influencing fertility for women.
Egg freezing is the only treatment currently available to preserve egg health
There’s no “anti-aging” treatment for your eggs (yet!). The only option available to women today who want to proactively preserve their fertility—and increase their chances of having a baby later in life—is to freeze their eggs or embryos.
Extend Fertility is the industry leader in egg freezing.
More women freeze their eggs at Extend Fertility than anywhere else in the country. We’ve frozen over 27,000 eggs in 2,500 cycles since we opened in 2016. We’re ready to talk to you about taking the next step toward preserving your fertility—and your options.