Should I get the COVID-19 vaccine if I’m trying to conceive, doing fertility treatment, or already pregnant?
As COVID-19 vaccination rollout continues across the country, many women who are trying to conceive, in the midst of fertility treatment, or already pregnant are wondering if the vaccine is right for them. While it’s ultimately a personal choice, we’ve gathered the important data and guidance to help you make an informed decision.
How do the COVID-19 vaccines work?
The two vaccines currently approved for emergency use in the US come from Pfizer and Moderna. Both are mRNA vaccines, which work a little differently than many other vaccines.
Typically, a vaccine contains a virus, or part of a virus, that’s either dead or has been weakened, so it can’t actually make you sick. When you inject the vaccine, your immune system springs into action, creating antibodies that fight off the virus. That defense is then stored as a kind of “muscle memory” that can be quickly and easily activated in the case that your immune system experiences the same virus again.
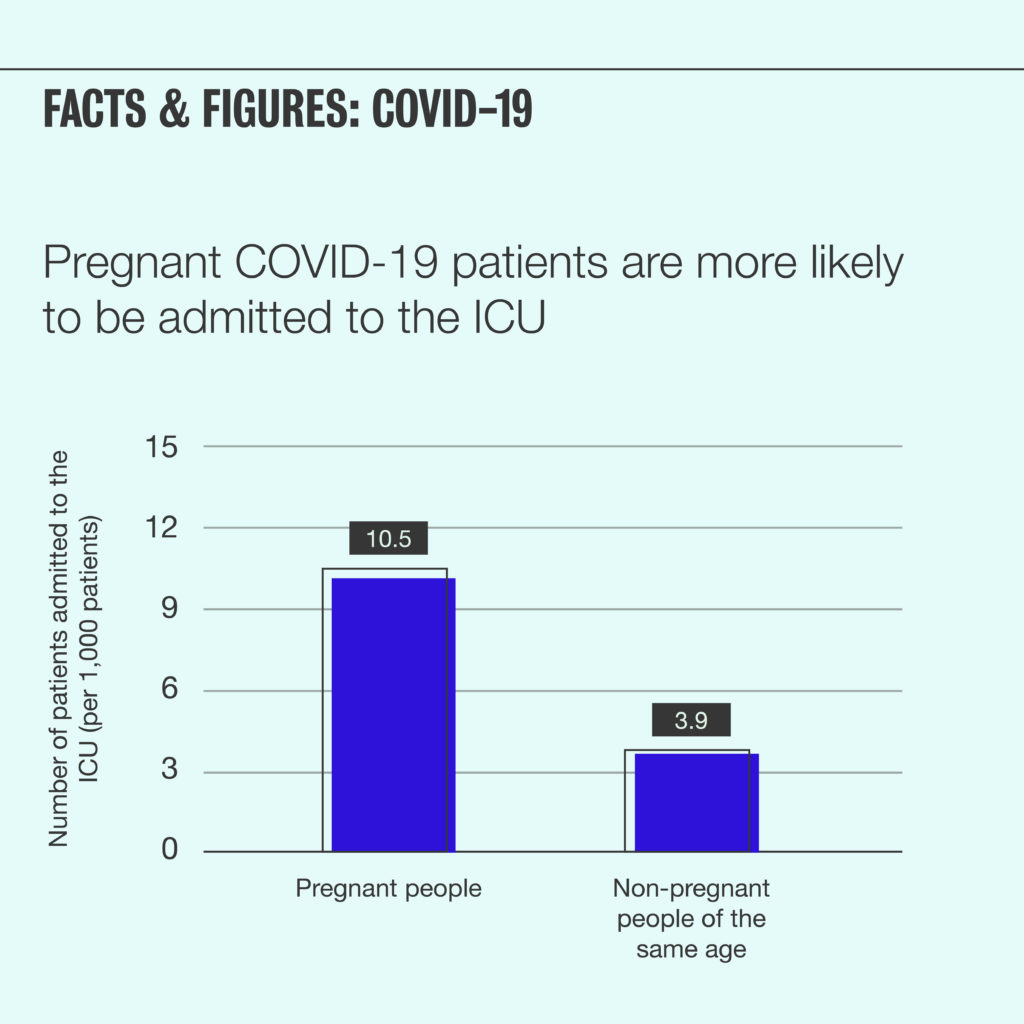
An mRNA vaccine, instead, contains a small piece of genetic code that instructs your cells to create a harmless protein that’s a lookalike for the “spike” protein on the outside of the coronavirus. Just as in the case of a traditional vaccine, the immune system recognizes this spike protein as foreign and creates antibodies to defend against it. The mRNA quickly degrades, but the immune response is “saved” in case of future exposure to a virus with the same spike. (The mRNA in the vaccine does not have the ability to enter your cells’ nucleus, where DNA is stored, and cannot alter or affect your body’s DNA in any way.)
One benefit of an mRNA vaccine is that it can allow you to build immunity against a virus without ever being exposed to the virus, even in a dead or weak form. And the Pfizer and Moderna COVID-19 vaccines are proving to be very effective. In trials of 30,000–40,000, these vaccines had around 95% efficacy. In layman’s terms, that means that unvaccinated people are 20 times more likely to get COVID-19 than vaccinated people. (See the Moderna Vaccine Brief or the Pfizer Vaccine Brief.)
Why is COVID-19 vaccination important for people who are pregnant or planning to become pregnant?
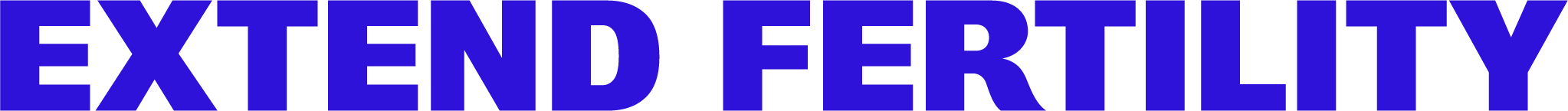
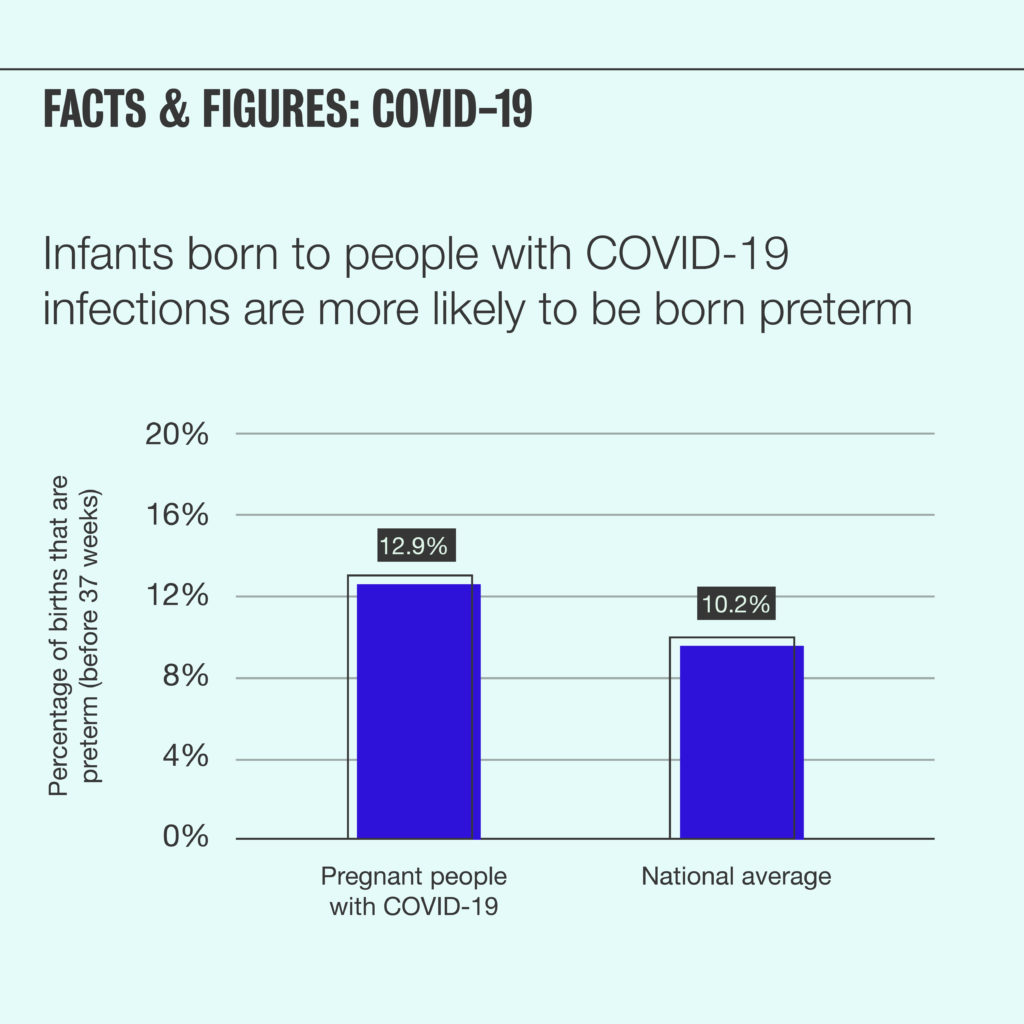
At this point in the pandemic, we know that COVID-19 infection can be more severe for pregnant people. According to the Center for Disease Control (CDC), pregnant COVID-19 patients are more likely to experience severe illness than non-pregnant patients of the same age. Additionally, preterm birth is more common among pregnant people infected with COVID-19 than among healthy pregnant people.
Given these statistics, the CDC has stated that pregnant people are in an “increased risk” category with regard to COVID-19. Vaccination is one of the best tools available to prevent infection.
Have the COVID-19 vaccinations been expressly tested on pregnant people?
No, but that’s not unusual. Pregnant people are rarely included in initial drug or vaccine trials. However, there’s nothing about the Pfizer or Moderna vaccines—not their ingredients, nor how they work—that’s raising concerns among OB/GYNs or maternal/fetal medicine experts. That’s why the FDA has left the decision to vaccinate up to individual women and their doctors.
According to the American College of Obstetricians and Gynecologists (ACOG), “based on the mechanism of action of these vaccines and the demonstrated safety and efficacy in clinical trials, it is expected that the safety and efficacy profile of the vaccine for pregnant individuals would be similar to that observed in non-pregnant individuals.” In other words, they believe the vaccine will be just as safe and effective for pregnant people as it is for their non-pregnant counterparts.
At this point in the vaccination effort, many pregnant people have been vaccinated without reported adverse effects. The vaccines will continue to be monitored for long-term impacts.
Should I get the COVID-19 vaccine if I’m planning to get pregnant?
The American Society for Reproductive Medicine (ASRM), the leading organization for the fertility field, recommends vaccination for people who are trying to or planning to conceive. Because the vaccine does not contain any actual virus, there is no reason to delay pregnancy attempts after vaccination.
Should I get the COVID-19 vaccine if I’m undergoing fertility treatment, like IVF or egg freezing?
According to the ASRM, patients undergoing fertility treatment should be encouraged to receive a COVID-19 vaccine when it’s available to them. There’s no evidence that vaccination before or during fertility treatment will impact the outcome of treatment in any way.
Should I get the COVID-19 vaccine if I’m pregnant?
Several pregnancy and fertility healthcare provider organizations, including ACOG, ASRM, and the Society for Maternal-Fetal Medicine (SMFM), recommend COVID-19 vaccination during pregnancy.
Specifically: ACOG states that “COVID-19 vaccines should not be withheld from pregnant individuals who meet criteria for vaccination.” Similarly, ASRM states that “pregnant patients should be encouraged to receive vaccination based on eligibility criteria.” SMFM “strongly recommends that pregnant and lactating people have access to the COVID-19 vaccines.”
Because COVID-19 vaccines don’t contain any actual virus, they’re not thought to cause an increased risk for first or second trimester loss, stillbirth, or congenital anomalies, according to ASRM.
While trials and common medical knowledge indicate that there are no strong safety concerns for vaccination in pregnant people, patients should discuss the available data with their doctor and weigh the risks and benefits of vaccination, including their potential exposure to COVID-19.
Will the COVID-19 vaccines affect fertility?
There is no evidence or indication that vaccination with an mRNA vaccine will impact future fertility. ACOG states that “Given the mechanism of action and the safety profile of the vaccine in non-pregnant individuals, COVID-19 mRNA vaccines are not thought to cause an increased risk of infertility.” ASRM concurs.
Additionally, though pregnant people were excluded from the initial trials, there were several patients who got pregnant during vaccine testing. In the Pfizer trial, 23 women got pregnant (12 from the vaccine group, and 11 from the placebo group); none of the women who had received a vaccine experienced a subsequent adverse pregnancy outcome. Similarly, in the Moderna trial, 13 pregnancies were reported (6 in the vaccine group, and 7 in the placebo group), with no adverse outcomes in the vaccine group pregnancies. While these numbers are still small, they point to a similar rate of pregnancy among vaccinated and unvaccinated women.
But what about that whole “vaccines will cause infertility” thing?
Unfortunately, there was a widely spread myth that the COVID-19 vaccine would cause infertility by creating antibodies that mistakenly attack a protein that’s crucial to the formation of the placenta, called syncytin-1, because it has some small genetic similarities to the coronavirus spike protein. There is no biological or evidence-based reason to believe this to be true, and it’s since been debunked by many experts.
More questions? Contact us.